Upon receiving treatment for their motor symptoms, many patients with Parkinson’s disease develop unwanted behavioral changes such as gambling addiction, excessive shopping, or compulsive eating. A common factor in these behaviors is a reduced ability to control own immediate impulses. Because these effects are often associated with shame, the problems have long been underreported and have remained largely unexplored. Now, researchers present how Parkinson´s medications can produce impulsive-compulsive behaviors by activating specific brain regions.
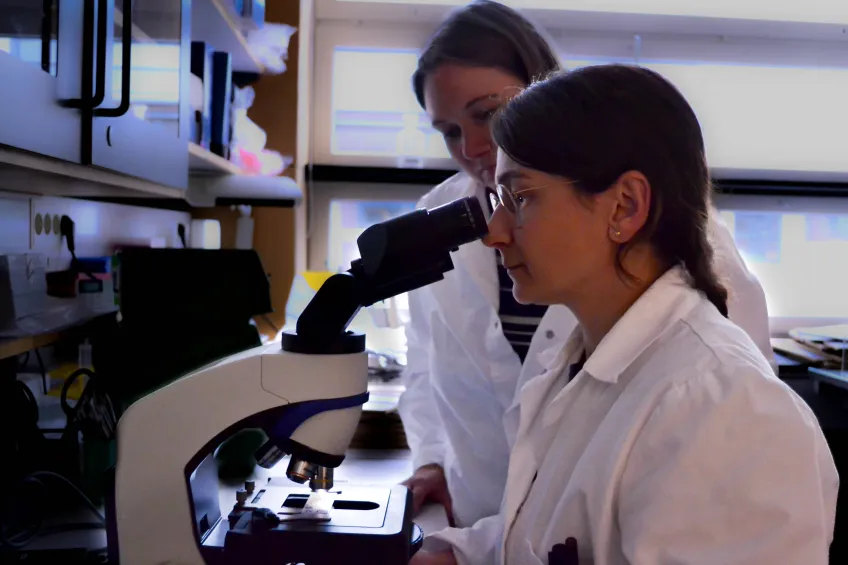
The study was conducted in a rat model of Parkinson’s as a part of the doctoral work of newly graduated Mirjam Wolfschlag. The project involves several research groups within the strategic research area MultiPark. In addition to experimental investigations, the thesis also includes epidemiological studies involving Parkinson’s patients.
In our patient studies, those who developed impulse control disorders were more frequently treated with dopamine agonists. But we lacked an explanation for why,explains Mirjam Wolfschlag.
“In our patient studies, those who developed impulse control disorders were more frequently treated with dopamine agonists, medications that bind specifically to certain types of dopamine receptors. But we lacked an explanation for why that led to reduced impulse control,” explains Mirjam Wolfschlag.
Since Parkinson’s disease causes dopamine loss in the part of the brain that controls movement, patients are treated with medications that compensate for this loss by activating dopamine receptors on the surface of nerve cells. Two common treatments are L-DOPA and ropinirole. L-DOPA is converted to dopamine in the brain and then activates all types of dopamine receptors, while ropinirole is one of the so-called dopamine agonists that primarily activate the D2 and D3 dopamine receptor types.
Dopamine not only controls movement but also motivation and decision-making, functions that influence our personality. Therefore, dopamine treatment can be associated with effects at several levels. A known issue with L-DOPA treatment is that it can cause involuntary movements, known as dyskinesia. Additionally, the dosage plays a significant role, which becomes increasingly difficult to manage as the disease progresses.
To understand how the different medications activate the brain, the researchers used a rat model of the disease. These animals were treated with L-DOPA, ropinirole, or a combination of both. Then, they used several new tests to measure impulse control and decision-making. In the rats treated with ropinirole, the tests revealed clear problems with impulse control and decision-making, and an appearance of behaviors with compulsive features . In contrast, L-DOPA did not produce any of such issues. Administering both drugs together did not worsen the problems caused by ropinirole; in fact, the issues seemed to be mitigated in one of the tests.
This activation pattern explains why dopamine agonists like ropinirole can impair impulse control and decision-making, explains Elena Espa.
“Compared to L-DOPA, ropinirole activated deeper centromedial parts of the striatum. The same striatal area is activated by addictive substances such as cocaine. This activation pattern explains why dopamine agonists like ropinirole can impair impulse control and decision-making, as these aspects are governed mostly by these parts of the striatum, whereas motor control is regulated in the more dorsolateral, superficial regions,” explains Elena Espa, who conducted the experiments together with Mirjam Wolfschlag.
Although the results show that ropinirole and similar drugs have adverse behavioral effects, excluding dopamine agonists and treating Parkinson’s patients only with L-DOPA is not a viable solution. The research group’s previous projects have shown that higher doses of L-DOPA lead to severe involuntary movements.
Our results suggest that L-DOPA could be combined with dopamine agonists to allow for lower doses of both medications, thereby reducing the risk of unwanted effects, concludes Professor Angela Cenci Nilsson.
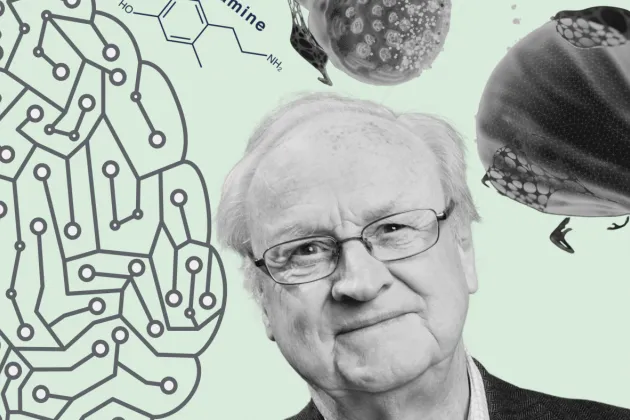
“Most unwanted effects of medications arise at higher doses. Overall, our results suggest that L-DOPA could be combined with dopamine agonists to allow for lower doses of both medications, thereby reducing the risk of unwanted effects at two levels, that is, involuntary movements and impulse control disorders. This potential needs to be further investigated in patients,” concludes Professor Angela Cenci Nilsson, senior author of the study.